Disc Replacement Surgery
- At least 90% of Americans will develop lower back pain at some point in time in their lives. 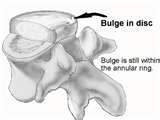 An estimated one million Americans suffer from a specific type of chronic back pain attributed to damage to discs of the spine. Pain caused by damaged discs in the spine is complex and not completely understood.
An estimated one million Americans suffer from a specific type of chronic back pain attributed to damage to discs of the spine. Pain caused by damaged discs in the spine is complex and not completely understood.
Disc replacement surgery is an exciting and relatively new surgical technique in the treatment of patients with disco genic back pain. Its advantages include a less destructive approach than posterior surgery, with the potential to maintain motion and protect the adjacent levels of the spine, by preventing a stress riser at the interface of the fusion.
Spinal fusion on the other hand is the gold standard by which new treatments must be measured. Spinal fusion has been used for more than 50-years and the long-term results are well understood and are generally reliable.
While disc replacement offers many potential advantages, it has not been shown to be superior to spinal fusion in randomized, controlled trials, although the postoperative recovery is certainly more rapid. The majority of the patients in this group are relatively young, certainly less than 60-years old, with many years to live. We have little idea about the long-term results of disc replacement and the possible complications which might occur in the future. We do know that revision surgery after disc replacement can be hazardous.
Surgeons and the public are inevitably enthusiastic about new developments, which have potential advantages, but caution needs to be exercised until long-term results of well-controlled trials are available.
The lumbar disc is a complex and beautifully adapted structure that must meet several conflicting requirements. The spine is flexible and the disc must allow movement while at the same time promoting stability and maintaining normal alignment. It must absorb excessive stresses and loads while distributing and transmitting forces through the trunk. Over time, these repetitive mechanical stresses and the aging process lead to a slow biochemical degradation of the disc. This is a natural process, occurring gradually in most people and usually goes largely unnoticed. However, for some, the process can result in pain and occasionally, neurological compromise. Most of these individuals can be treated successfully without recourse to surgery. For a few, however, their symptoms of back pain remain very intrusive and impose unacceptable functional restrictions. The spinal surgeon is then looked to for a response.
Traditionally, the response has been to fuse the affected part of the spine. Fusion has become, the gold standard in the surgical treatment of degenerative disease in the lumbar spine, although it is debatable whether it deserves such a lofty status.
Spinal fusion emerged early in the last century as a means of dealing with spinal infection, later being extended to fractures and tumors, and then to cases of spinal deformity. The intention was to restore segmental stability and spinal alignment. Spinal fusion for degenerative disease is a relatively recent extension of the indications for this technique. Nonetheless, it is one which became established by default, in the absence of any viable alternative.
Spinal fusion is an expensive procedure entailing a long hospital stay. It has a significant rate of complications and considerable morbidity. Recuperation is lengthy and slow, and return to work considerably delayed. The posterior approach to the spine inevitably causes damage to the para vertebral muscles which are so important in subsequent functional recovery. Harvesting autogenous bone from the pelvis, for which there is no satisfactory substitute, can cause chronic donor site pain. Failure of fusion remains a problem even with the use of sophisticated instrumentation.
The use of screws and cages has appreciable neurological and vascular risks. The reported incidence of these complications varies, but a meta-analysis of 47 publications found a 9% risk of significant donor site pain and a pseudarthrosis rate of 14%.
A particular concern with rigid fusion is the transfer of stress to adjacent segments. This may cause symptomatic degenerative disease in the long term, which can progress to a severity requiring further surgery in up to 20% of patients. and perhaps even 37%, within a decade following ‘successful’ lumbar fusion. This risk may lead to the exclusion of many very deserving patients from consideration for surgery if the adjacent segments show any existing sign of degeneration, even if this is asymptomatic. Success with spinal fusion certainly relies on robust and stringent patient selection, but for these patients this is effectively an admission of failure.
Given the risks, morbidity and limited application of spinal fusion it's not surprising that spinal surgeons have looked over the shoulders of their colleagues undertaking successful hip and knee arthroplasty, and sought to emulate this success through more physiologically sound procedures. Various non rigid stabilization techniques and arthroplasty solutions have been developed, of which disc replacement is among the most important.
Surgical Technique
Accurate central placement of the prosthesis is a critical determinant of outcome and requires midline anterior access to the appropriate level. This can be achieved through a 5–7 cm transverse incision, splitting the rectus muscles. Finger dissection around the retro peritoneal space quickly gains access to the appropriate level of the spine. The pre-sacral nerves come forwards with the peritoneum minimizing the risk of retrograde ejaculation. The common iliac vessels can be retracted to give wide exposure of the lumbo-sacral disc. The L4/L5 disc is at or above the level at which the great vessels bifurcate and these must, therefore, be mobilized over to the right, after first ligating and dividing the iliolumbar vein.
The pre-sacral nerves come forwards with the peritoneum minimizing the risk of retrograde ejaculation. The common iliac vessels can be retracted to give wide exposure of the lumbo-sacral disc. The L4/L5 disc is at or above the level at which the great vessels bifurcate and these must, therefore, be mobilized over to the right, after first ligating and dividing the iliolumbar vein.
The disc is excised, clearing particularly the posterior annulus to facilitate mobility of the artificial disc. The cartilaginous end plates are scraped clean, although preserving the bony end plates upon which the prosthesis will rest. Sizing of the prosthesis is established with trials and the prosthesis is then accurately positioned using radiographic guidance. Immediate fixation is achieved through teeth or a keel on the prosthetic end plates, and may be enhanced subsequently by bony in-growth into a porous coating.
Following surgery, patients can be mobilized quickly and are remarkably comfortable from the outset. Physiotherapy helps to enhance muscle stability but no brace is required. The patient can go home after 3–4 days on light activities and generally returns to work within 3–4 weeks. Fitness training is allowed from 6 weeks and patients can return to sports within 2–3 months.
Benefits for Patient from Surgery
Several advantages of disc replacement are self-evident. No bone graft is taken so there is no risk of donor site pain. Similarly, none of the problems associated with failure of fusion will occur. These problems may require revision surgery, often with poor results.
Patients undergoing disc replacement improve substantially faster following surgery. This is perhaps because there is virtually no muscle trauma and indeed there is none of the other ‘collateral damage’ seen in spinal fusion. Their hospital stay is shorter and patients need little in the way of social and functional support following surgery. This is in stark contrast to the course after spinal fusion, and comes as quite a surprise to patients (and their GPs) who have often been ‘warned’ what to expect with spinal surgery. In terms of symptoms, it takes 6–12 months for fusion patients to achieve the same improvement seen by 6 weeks in those undergoing disc replacement. A similar pattern is seen in functional outcome. The importance of this very significant ‘head start’ should not be underestimated. Many of these patients have suffered for years from disabling back pain, often having tried, and failed, many forms of treatment. This rapid and dramatic improvement instills a belief and confidence that allows them to get their lives back on track.
Any exciting new procedure inevitably raises expectations of dramatically improved results. However, a well-performed spinal fusion can achieve a satisfactory medium-term clinical outcome in a good proportion of carefully selected patients. It is, therefore, perhaps unrealistic to expect a dramatic difference between the two techniques, at least in the first few years, once the early gains from the less damaging surgery of disc replacement are passed.
Both procedures deal effectively with the patient's principal pain source. The movement allowed by disc replacement may confer some clinical benefit. Similarly, the long-term effects of ‘collateral damage’ may continue to mar the results from spinal fusion, and problems resulting from a failure of fusion may reduce the results for this group a little further. As such, the outcome measures from the various clinical trials at 2 years have shown either a moderate but significant benefit with total disc replacement, with the two techniques. Even so, patient satisfaction is considerably greater: 92% of disc replacement patients indicated that they would definitely undergo the same procedure again. Only 55% of fusion patients felt the same.
One of the principal potential advantages of disc replacement, the avoidance of adjacent level problems, must await longer term comparative studies. Several such studies have been commenced, comparing disc replacement with fusion in various guises. It may take over a decade for junctional changes to evolve following fusion and thus for this advantage of motion preservation to become apparent. Needless to say, a definitive answer to this question is keenly awaited. Click for health tip of the day.
Eliminating stress transfer to adjacent levels may also enhance possible indications for intervention. Many patients who previously were denied surgery because of mild changes at other levels of the lumbar spine may now be candidates, while others, who might previously have been offered a multilevel spinal fusion, could benefit from less extensive motion preserving techniques.