Charcot Foot
Diagnosis and Definition of Charcot Foot
 A good time to start taking better care of your feet is today
and possibly you may avoid getting charcot foot, or possibly heal the condition...
Charcot foot is described as neuroarthropathy of the foot, which
typically manifests in the forefoot, mid foot and ankle region. This
presents as hot red swollen foot that may be misdiagnosed as an infection
or gout in the early phase with or without mid foot collapse.
A good time to start taking better care of your feet is today
and possibly you may avoid getting charcot foot, or possibly heal the condition...
Charcot foot is described as neuroarthropathy of the foot, which
typically manifests in the forefoot, mid foot and ankle region. This
presents as hot red swollen foot that may be misdiagnosed as an infection
or gout in the early phase with or without mid foot collapse.
Initial Diagnosis and Management
• Red, hot swollen foot
• Sudden onset of inflammation with warmth and edema, and erythema
of the foot without a break in the skin or known point of entry for
infection
Charcot foot generally presents with the following symptoms:
• Neuropathy, or loss of sensation to foot
• History of diabetes, anaemias, ETOH,
severe or moderate rheumatoid arthritis or
other autoimmune disorders
• Symptoms of acute injury without known incident (i.e. red,
hot, swollen foot)
• Will have good arterial flow, i.e. good pedal pulses
Charcot foot may or may not have the following symptoms:
• Pain in the affected foot
• No evidence of osteomyelitis
• Gross foot deformity
• History of or loss of foot architecture, i.e. mid foot collapse,
severe lowering of foot arch
• Arthropathy affecting lower extremity
• During acute onset, charcot may have negative x-ray or bone scan
• During mid to late stages, may have obvious shards of bone
or fracture
Labs
• ESR elevation
• Absent WBC elevation
• Baseline HbA1c of value in diabetic
Treatment of Charcot Foot
• Non-weight bearing on affected lower extremity until diagnosis confirmed.
Ongoing Management and Objectives of Charcot Foot
• To decrease the rate of toe, foot and lower extremity amputation
with prompt referral of suspected charcot feet, or active
 foot ulcerations
foot ulcerations
• To manage each patient’s condition with a combination
of mechanical, medical and surgical therapies tailored specifically
for the unique characteristics of neuroarthropathy with/without ulcerations
Indications for Specialty Care Referral
All patients with suspected Charcot foot should be treated only by specialist care from a foot-care doctor or by chiropodists who deals with diabetic patients and the problems associated with feet. All charcot-foot patients should be followed-up by the primary care provider for treatment of all co-morbid conditions and routine foot-care with the goal of optimal health & wellness for the charcot patient
High Risk Diabetic Foot Evaluation Referral Guideline
High risk diabetic foot is a general term used to describe a variety
of foot problems related to diabetes mellitus that may result in limb
loss if unmanaged.
 These complications range from skin fissures to
large non-healing feet ulcers that commonly originate from shoe related
blisters or unidentified trauma and may potentially lead to amputation.
Other factors that contribute to diabetic foot complications include:
peripheral neuropathy (light touch, motor and autonomic), deep or
superficial infections, structural changes and deformities (i.e.,
hammertoes, bunions, osseous prominences, Charcot joint, etc.), arterial
and venous insufficiency, traumatic foot or ankle injury, or due to a foreign body.
These complications range from skin fissures to
large non-healing feet ulcers that commonly originate from shoe related
blisters or unidentified trauma and may potentially lead to amputation.
Other factors that contribute to diabetic foot complications include:
peripheral neuropathy (light touch, motor and autonomic), deep or
superficial infections, structural changes and deformities (i.e.,
hammertoes, bunions, osseous prominences, Charcot joint, etc.), arterial
and venous insufficiency, traumatic foot or ankle injury, or due to a foreign body.
Initial Diagnosis and Management
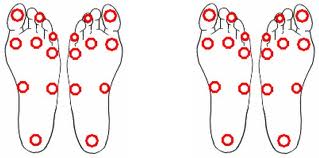
Below are the Risk Factors for the Charcot Foot:
1. Vascular disease or history of re vascularization or interventional procedure(s)
2. History of lower extremity ulcer and/or lower extremity infection
3. Partial foot/toe amputation or contralateral limb/ leg amputation
4. Peripheral or diabetic neuropathy medical conditions.
- A. Burning, tingling, numbness, or hyperesthesia unresponsive to tight glycemic control
- B. Drop foot deformity not controlled with a brace/ shoe gear changes
- C. Absent sensation in part or entire foot to include distal leg
5. Inability to find shoes which fit due to deformity, recurrent shoe gear related ulcerations, instability, or sensitivity.
Physical assessment of the foot to include: 
1. Ulceration
2. Skin fissures
3. Presence of hemorrhagic hyperkeratotic tissue, excessive blisters
4. Absence of pedal pulses
5. Loss of protective threshold diagnosed with monofilament and vibratory testing
6. Foot deformity
7. Compromised nutritional status
8. End stage renal disease
9. Signs of lower extremity infection
10. Pallor of lower extremity on elevation and rubor of lower extremity on dependency
11. Maceration within digital web spaces
12. Charcot foot
Ongoing Management and Objectives
To decrease the rate of toe, foot, and lower extremity amputation
in the diabetic population with referral of those patients considered
to be at high risk for developing ulceration, infection, and Charcot
foot deformities, to a group of extremity specialists
 who focus on mechanical, medical, and surgical intervention in the treatment of the diabetic
foot and lower extremity.
who focus on mechanical, medical, and surgical intervention in the treatment of the diabetic
foot and lower extremity.
Indications for Specialty Care Referral
Patients with any of the following should be referred to the LIMB PRESERVATION SERVICE/ WOUND CARE CLINIC:
Any diabetic patient with ulcerations, signs of foot infection, traumatic injury, presence of a foreign body or suspected charcot foot should be referred as an ASAP. Click-here for Health Tip-of-the-Day.
Patients with a combination of one or more of the signs and symptoms identified in the Initial Diagnosis and Management above should be referred as potential high risk to Mary Anne Landowski, RN who will perform a detailed foot evaluation and arrange for appropriate care.
Criteria for Return to Primary Care
After any acute extremity related problem has been appropriately treated.
Patients found to be at high risk for foot ulcerations should be followed in the Limb Preservation Service at intervals determined by the clinic providers in conjunction with the Primary Care Provider. These follow-up intervals will change based upon the progression or regression of the complications identified in each specific patient.
All patients should be followed by the primary care provider for treatment of all co-morbid conditions and routine care with the goal of optimal health and wellness for the whole patient.
Footwear
 Improper or poorly fitting shoes are major contributors to diabetes
foot ulcerations. Counsel patients about appropriate footwear. Patients
with diabetes need to pay special attention to the fit and style of
their shoes and should avoid pointed-toe shoes or high heels. Properly fitted and comfortable athletic, or quality walking shoes and sandals are highly recommended for daily foot-wear. If off-the-shelf shoes are used, make sure there is room to accommodate
any foot deformities.
Improper or poorly fitting shoes are major contributors to diabetes
foot ulcerations. Counsel patients about appropriate footwear. Patients
with diabetes need to pay special attention to the fit and style of
their shoes and should avoid pointed-toe shoes or high heels. Properly fitted and comfortable athletic, or quality walking shoes and sandals are highly recommended for daily foot-wear. If off-the-shelf shoes are used, make sure there is room to accommodate
any foot deformities.

